Pediatric Critical Care
Like adults, when a child has life-threatening symptoms or an unstable condition, they need special attention. A child may not be able to fight diseases and recover from health conditions the same way an adult can. So, medical care that specifically focuses on the child’s medical needs is crucial for recovery.
Stormont Vail’s Pediatric Intensive Care team includes highly skilled specialists to provide dedicated and uninterrupted care to children and teens.
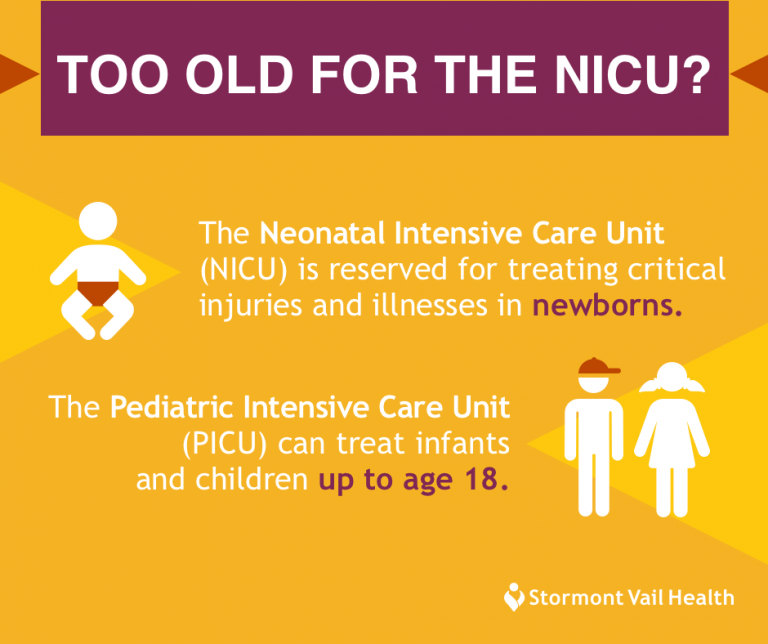
Pediatric Intensive Care Unit (PICU) at Stormont Vail Health
The Pediatric Intensive Care Unit (PICU) offers one procedure room, with additional equipment, and 15 private rooms with secure entry to ensure the utmost safety. The PICU has a full interdisciplinary team of professionals that works with families and children every day. We have team rounds including Pediatric Intensivist, Pediatric Pharmacist, Child Life, Social work, and Case Management, who involve the family in important decision making and planning. This well-supported team also includes a group of pediatric experts and sub-specialty doctors including pediatric neurologists, pediatric endocrinologists, pediatric hematology/ oncologists, pediatric cardiologists, and other surgical service professionals.
Conditions We Treat
Medical and surgical pediatric conditions most commonly treated in pediatric intensive care include:
Treatment Options
Our pediatric intensivists — specialists certified in pediatric critical care — provide care such as:
Evaluating a child’s condition and making a diagnosis
Prescribing medications and outlining treatment plans for children with lung disease and brain trauma
Monitoring the child’s condition around the clock
Placing catheters in the blood vessels and heart to examine if the heart is working well
Stormont Vail Health and Children’s Mercy Kansas City Announce Expanded Partnership

Stormont Vail Health and Children’s Mercy Kansas City are expanding their ongoing relationship that provides pediatric specialty services for children and families in Topeka and surrounding areas by opening a new dedicated pediatric clinic in Topeka-Children’s Mercy Topeka at Stormont Vail Health. The new clinic is scheduled to open in October. The Children’s Mercy team…
Pediatric Intensivist Satish Shah, M.D., Joins Stormont Vail Health

Stormont Vail Health is proud to announce that Satish Shah, M.D., has joined our medical team and will practice as a Pediatric Intensivist, located at 1500 SW 10th Ave., Topeka, Kan. 66606. Dr. Shah will work in intensive care units or emergency rooms, providing emergency medical care to children. Dr. Shah’s approach to medicine is…
Resources For Families
We believe family plays a central role in a child’s recovery, which is why we involve the patient’s family in the treatment plan. We update you on your child’s condition, educate you on providing care for your child, and offer emotional support. We have multiple resources available for families including:
Child Life Program to offer play-based methods of support for children
Daily bedside meetings with the patient, family, and full team of care providers
Ronald McDonald House to accommodate out-of-town families
Flexible visiting hours for families: Parents are able to be at the bedside 24/7. Other visitors can come to see a patient between 9 a.m. and 9 p.m.
Grief and loss support
Customized Baby Care Education Classes



